Basic and Clinical Anatomy Details
Basic and Clinical Anatomy. Mobile Phone 01797522136, 01987073965. Basic anatomy is the part of anatomy that should be known to everyone in medical science. Clinical anatomy is part of anatomy that focuses on medical diagnosis and medical practice. So, basic anatomy is necessary for all medical students, and clinical anatomy is essential for medical practitioners. Here we discuss the Clinical Anatomy of the diaphragm, the Clinical Anatomy of Thoracic aorta, Branches of the thoracic aorta, mammary gland, and the Clinical Anatomy of the Heart.
Clinical Anatomy of The Right Atrium, Clinical Anatomy of The Left Atrium, Clinical Anatomy of The Right Ventricle, Clinical Anatomy of The Left Ventricle, Coronary Circulation, Nerves Supply to the Heart, The Bronchi, Blood Supply to the Lung, Clinical Anatomy of Abdominal Aorta, Mesenteric Artery, The Peritonium, Anatomy of the Spleen, Anatomy of the Pancreas, Anatomy of the Liver, Anatomy of Stomach, Anatomy of Colon, Anatomy of Rectum, Anatomy of Cecum, Anatomy of Anus.
This Subject is studied in some courses. These courses are Paramedical 3 Years, DMA 3 Years, DPM 3 Years, DMDS 4 Years, and DMSc 4 Years. All Courses are available at HRTD Medical Institute. HRTD Medical Institute is an Organization of HRTD Limited.
The Diaphragm
Dome-shaped septum separating the thorax from the abdomen Undergoes contraction and relaxation, altering the volume of the thoracic cavity and the lungs, producing inspiration and expiration
Clinical Anatomy of Thoracic Aorta
- The aorta can be divided into four sections: the ascending aorta, the aortic arch, the thoracic (descending) aorta, and the abdominal aorta
It terminates at the level of L4 by bifurcating into the left and right common iliac arteries
- The ascending aorta arises from the aortic orifice of the left ventricle and is 2 inches long. It gives the origin of the right and left coronary arteries
Branches of the thoracic aorta in descending order
- Bronchial arteries
- Mediastinal arteries
- Oesophageal arteries
- Pericardial arteries
- Superior phrenic arteries
- Intercostal and subcostal arteries
Clinical Anatomy of Mammary Gland
- The breast are paired structures located on the anterior thoracic wall, in the pectoral region
- They are present in both males and females following puberty.
- The mammary glands are the key structures involved in location
The base of the breast lies on the pectoral fascia. It acts as an attachment point for the suspensory ligaments. There is a layer of loose connective tissue between the breast and pectoral fascia. known as the rectro mammary space. This is a potential space often used in reconstructive plastic surgery. At the center of the breast is the nipple composed mostly of smooth muscle fibers. Surrounding the nipple is a pigmented area of skin termed the areole. There are numerous sebaceous glands within the areolae that enlarge during pregnancy secreting an oily substance that acts as a protective lubricant for the nipple.
Clinical Anatomy of Heart
The heart is a hollow muscular pump, which lies in the middle mediastinum. The right heart circulates blood to the lungs where is oxygenated, and the left heart receives this and circulates it to the rest of the body.
In its typical anatomical orientation, the heart has 5 surfaces
- Anterior right ventricle
- Posterior left atrium
- Inferior Left and right ventricle
- Right pulmonary -Right atrium
- Left pulmonary- left ventricle
Separating the surface of the heart are its borders
There are four main borders of the heart
- Right border-Right atrium
- Inferior border ventricle and right ventricle
- Left border -Left ventricle
- Superior border -Right and left atrium and left atrium the great vessels
The right atrium
- The right atrium receives deoxygenated blood from the superior and inferior vena cava
- It also receives drainage from the coronary veins the coronary sinus
- The atrium pumps this blood to the right ventricle.
Tributaries of the right atrium
- Superior venacava (svc)
- Inferior venacava(Ivc)
- Coronary sinus
- Anterior cardiac veins
- Venae cordis minimi (Thebesian veins)
- Sometimes, the right marginal vein.
The left atrium
- The left atrium receives oxygenated blood from the pulmonary veins
- In the anatomical position,it forms the posterior border of the heart
- blood is pumped from the left atrium into the left ventricle
Much like the right, the left atrium can be divided embryologically
Inflow portion – this part receives blood from the pulmonary veins. Its internal surface is smooth. It is derived from the pulmonary veins themselves
Outflow portion – This part is located anteriorly, where the blood flows into the ventricles. It contains the pectinate muscles and the left auricle. It is derived from the embryonic atrium
The right ventricle(RV)
- The right ventricle receives deoxygenated blood from the right atrium and pumps it into the pulmonary artery
- The ventricle is triangular in shape and forms the majority of the anterior border of the heart
Interior of the right ventricle
- The interior of the inflow part of the right ventricle is covered by irregular muscular structures, called trabeculae carneae. They give the ventricle a ‘sponge-like’ appearance
- The outflow part (leading to the pulmonary artery) is located in the superior aspect of the ventricle. It is called the conus arteriosus and is derived from the embryonic bulbus cordis. It is visibly different from the rest of the ventricle, having smooth walls, with no trabeculae carneae
Clinical Anatomy of The Left Ventricle (LV)
The left ventricle receives oxygenated blood from the left atrium and expels it into the aorta
It is located anteriorly to the left atrium, contributing to the anterior aspect of the heart, and forming the apex
In the left ventricle, there are two papillary muscles, which are larger than those found in the right. They are attached to the chordae tendinae, which in turn attach to the mitral valve
Interior of the left ventricle
- The interior surface of the left ventricle contains trabeculae carnea, in a similar structure to that of the right
- The outflow part of the left ventricle is known as the aortic vestibule. It is smooth- walled, and a derivative of the embryonic bulbus cordis
The coronary circulation
- The left main and right coronary arteries arise from the left and right sinuses of the aortic root (distal to the aortic valve)
- The coronary anatomy varies greatly from person to person and there are many ‘normal variants’
- Coronary blood vessels receive sympathetic and parasympathetic innervations
- Stimulation of a-adrenoreceptors causes vasoconstriction (but the predominant effect is hypoxic vasodilatation)
- Stimulation of ẞ2-adrenoreceptors causes vasodilatation Parasympathetic stimulation also causes modest vasodilatation
Nerve supply of the heart
- The normal sinus rhythm and the heart rate are influenced by the autonomic nervous system through sympathetic and parasympathetic nerves
- These arise from two paired cardiovascular centers in the medulla oblongata
- The vagus nerve of the parasympathetic nervous system acts to decrease the heart rate, and nerves from the sympathetic trunk act to increase the heart rate. These come together in the cardiac plexus near the base of the heart
- Without parasympathetic input which normally predominates, the sinoatrial node would generate a heart rate of about 100 bpm
- The nerves from the sympathetic trunk emerge through the T1-T4 thoracic ganglia and travel to both the sinoatrial and atrioventricular nodes, as well as to the atria and ventricles
- The ventricles are more richly innervated by sympathetic fibers.
Clinical Anatomy of The Bronchi
- At the level of the sternal angle, the trachea bifurcates into the right and left main bronchi.
- Right main bronchus -widwer, shorter, and descends more vertically than its left-sided counterpart. clinically, this results in a higher incidence of foreign body inhalation.
The structure of bronchi is very similar to that of the trachea, though differences are seen in the shape of their cartilage.
- In the main bronchi, cartilage rings completely encircle the lumen.
- However, in the smaller lobar and segmental bronchi cartilage is found only in crescent shapes.
The bronchi derive innervation from T2-4 segment of the spinal cord and pulmonary branches of the vagus nerve. Blood supply to the bronchi is form branches of the bronchial arteries, while venous drainage is into the bronchial veins.
Clinical Anatomy of Bronchioles
- The smallest airways, bronchioles do not contain any cartilage or mucus-secreting goblet cells
- Instead, Clara cells produce a surfactant lipoprotein which is instrumental in preventing the walls of the small airways from sticking together during expiration
- Initially, there are many generations of conducting bronchioles, which transport air but lack glands and are not involved in gas exchange
- Conducting bronchioles then eventually end as terminal bronchioles These terminal bronchioles branch even further into respiratory bronchioles, which are distinguishable by the presence of alveoli extending from their lumens.
Clinical Anatomy of Alveoli
- Alveoli are tiny air-filled pockets with thin walls (simple squamous epithelium), and are the sites of gaseous exchange in the lungs
- Altogether there are around 300 million alveoli in adult lungs, providing a large surface area for adequate gas exchange
- The alveoli are located in the respiratory zone of the lungs
- Between neighboring alveoli lie thin interalveolar septa (which is vascularized with the richest capillary networks in the body, macrophages are also located in these septa)
- Alveolar pores (of Kohn) connect neighboring alveoli
- The alveoli contain some collagen and elastic fibers
- The elastic fibers allow the alveoli to stretch as they are filled with air during inhalation. They then spring back during exhalation in order to expel the carbon dioxide-rich air.
Clinical Anatomy of the Pleura
The pleura consists of a serous membrane that lines the lung and thoracic cavity.
Each pleura can be divided into two parts
- visceral pleura-covers the lung
- The parietal pleura covers the internal surface of the thoracic cavity.
The parietal pleura covers the internal of the thoracic cavity.
The parietal pleura covers the internal surface of the thoracic cavity. It is thicker than the visceral pleura and is subdivided into…
- Mediastinal pleura -covers the lateral aspect of the mediastinum.
- Cervical pleura -lines the extension of the pleural cavity into the neck.
- costal pleura covers the inner aspect of the ribs, costal cartilage, and intercostal muscles.
- Diaphragmatic pleura -covers the thoracic surface of the diaphragm.
Blood supply of the lungs
- The pulmonary trunk arises from the right ventricle
- Divides in front of the left main bronchus into right & left pulmonary arteries
- The right pulmonary artery divides into three branches one for each lobe of the right lung (which carries deoxygenated blood to the alveoli)
Clinical Anatomy of Abdominal Aorta
The abdominal aorta is a continuation of the thoracic aorta beginning at the level of the T12 vertebrae. It is approximately 13 cm long and ends at the level of the L4 vertebra. At this level, the aorta terminates by bifurcating into the right and left common iliac arteries that supply the lower body
Branches of abdominal aorta in descending order
- Inferior phrenic arteries: paired arteries arising posteriorly at the level of T12. They supply the diaphragm
- Coeliac artery: a large, unpaired visceral artery arising anteriorly at the level of L1. It is also known as the celiac trunk and supplies the liver, stomach, abdominal esophagus, spleen, superior duodenum, and the superior pancreas
- Superior mesenteric artery: a large, unpaired visceral artery arising anteriorly, just below the celiac artery. It supplies the distal duodenum, jejunum-ileum, ascending colon, and part of the transverse colon. It arises at the lower level of L1
- Middle suprarenal arteries: small paired visceral arteries that arise on either side posteriorly at the level of L1 to supply the adrenal glands
- Renal arteries: paired visceral arteries that arise laterally at the level between Ll and L2. They supply the kidneys.
Clinical Anatomy of The superior mesenteric artery
Is the second of the three major anterior branches of the abdominal aorta (the other two are the coeliac trunk and inferior mesenteric artery). It arises anteriorly from the abdominal aorta at the level of the L1 vertebrae, immediately inferior to the origin of the coeliac trunk
The superior mesenteric artery then gives rise to various branches that supply the small intestines, Loft cecum, ascending and part of the transverse colon
- Inferior pancreaticoduodenal artery
- Jejunal artery
- Ileal artery
- Ileocolic artery
- Right colic artery
- Middle colic artery.
Clinical Anatomy of The inferior mesenteric artery
Is the last of the three major anterior branches of the abdominal aorta. It arises at L3 near the inferior border of the duodenum,3-4 cm above where the aorta bifurcates into the inferior border of the duodenum,3-4 cm above where the aorta bifurcates into the common iliac arteries.
There are three mejor branches that aries from the IMA the left cardio artery, sigmoid artery, and superior rectal artery.
Clinical Anatomy of the Peritoneum
- The peritoneum is a continuous transparent membrane that lines the abdominal cavity and covers the abdominal organs.
- It acts to support the viscera and provides a pathway for blood vessels and lymph.
The peritoneum consists of two layers that are continuous with each other; the parietal peritoneum and the visceral peritoneum. They both consist of a layer of simple squamous epithelial cells, called mesothelium.
Parietal peritoneum
- The parietal peritoneum lines the internal surface of the abdominopelvic wall
- It is derived from somatic mesoderm in the embryo
- It receives the same somatic nerve supply as the region of the abdominal wall that it lines, therefore pain from the parietal peritoneum is well localised and it is sensitive to pressure, pain, laceration, and temperature
The peritoneal cavity
- The peritoneal cavity is a potential space between the parietal and visceral peritoneum
- It contains only a thin film of lubricating peritoneal fluid, which consists of water, electrolytes, leukocytes, and antibodies
- The peritoneal cavity can be divided into the greater and lesser peritoneal sacs (which communicate through epiploic foramen)
- The greater sac is constitutes the majority of the peritoneal cavity The lesser sac (also known as the omental bursa) is smaller and lies posterior to the stomach and lesser omentum.
Clinical Anatomy of Pancreas
- The pancreas is a 12-15-cm long J-shaped, soft, lobulated, retroperitoneal organ
- It lies transversely, although a bit obliquely, on the posterior abdominal wall behind the stomach, across the lumbar (L1- 2) spine
The pancreas is typically divided into 5 parts
- The head of the pancreas lies in the duodenal Cloop in front of the inferior vena cava (IVC) and the left renal vein
- The uncinate process is wedged between the superior mesenteric vessels in front and the norta behind it
- The Neck: located between the head and the body of the pancreas, It overlies the superior mesenteric vessels
- The Body: the body is centrally located, lie behind the stomach and to the left of the superior mesenteric vessels
- The Tail: the left end of the pancreas that lies within close proximity to the hilum of the spleen. It is contained within the splenorenal ligament with the splenic vessels. This is the only part of the pancreas that is Intra pe
Clinical Anatomy of the Spleen
The spleen is located in the upper left quadrant of the abdomen, under cover of the diaphragm and ribcage – and therefore cannot be palpated on clinical examination
- Lies relative to the 9th and 11th ribs
- The spleen is situated between the fundus of the stomach and the diaphragm
- It is an intraperitoneal organ, entirely surrounded by the peritoneum (except at the splenic hilum)
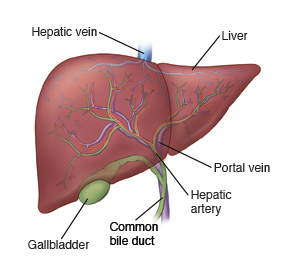
Clinical Anatomy of the liver
- Largest gland: 1600 g in male & 1300 g in female
- Five surfaces: anterior, posterior, superior, inferior & right
- The right lobe is much larger than the left lobe & forms five-sixths of the liver. It contributes to all 5 surfaces & presents the caudate & quadrate lobes
The liver is located in the right upper quadrant of the abdominal cavity just below the diaphragm. Anterior to the liver is the anterior abdominal wall and ribcage. Superior to the liver is the diaphragm. Posterior to the liver are the esophagus, stomach, gallbladder, and first part of the duodenum.
The surface of the liver is covered by visceral peritoneum (serosa), with a Glisson capsule underneath (blue area)
Clinical Anatomy of the Stomach
- The stomach is a digestive organ which extends between the levels of T7 and L3 vertebrae
- Within the GI tract, it is located between the esophagus and the duodenum
parts of stomach
Fundus
Cardia
Body Pylorus
The stomach has the shape of a J, and features a lesser and greater curvature. The stomach has four main regions: the cardia, fundus, body and pylorus The cardiac notch (incisura cardiaca gastri) is the acute angle between the abdominal esophagus and the fundus of the stomach
Clinical Anatomy of Duodenum
The duodenum is the widest and shortest part of the small intestine connecting the stomach to the jejunum. It begins with the duodenal bulb and ends at the suspensory muscle of the duodenum.
Anatomically, the duodenum is divided into four parts
- superior
- Descending
- Inferior
- ascending.
Together these parts form a C-shaped structure That wraps around the head of the pancreas. The first part of the duodenum lies within the peritoneum but its other parts are retroperitoneal.
Clinical Anatomy of the Large Intestine
Anatomically the large intestine can be split into several sections
- Cecum and appendix
- Colon
- Rectum
- Anal canal
The large intestine develops partly from the midgut (from cecum to distal transverse colon), Rectum the hindgut (from distal transverse colon to dentate line in anorectum), and proctodeum (below the dentate line)
The mucosa includes a columnar epithelium with a large number of mucus-secreting goblet cells (villi, which are present in the small intestine, are absent in colon), lamina propria (rich in lymphoid tissue), and muscularis mucosa. The submucosa contains the blood vessels and Meissner nerve plexus. The muscularis propria contains the inner circular and outer longitudinal muscles and myenteric (Auerbach) nerve plexus; teniae coli are formed by outer longitudinal muscles. The serosa of the colon is visceral peritoneum
Clinical Anatomy of the Caecum
- The cecum is the first part of the large intestine
- It is a blind-ended sac, continuous with the ascending colon, and lies in the right iliac fossa
- The terminal ileum opens into the cecum at its medial wall, and the opening is guarded by an ileocecal valve
Clinical Anatomy of Colon
The colon has four parts (1) the ascending colon (2) the transverse colon (3) descending colon and (4) the sigmoid colon. These sections form an arch, f gut encircling the small intestine. The transverse colon Ve extends from hepatic flexure to splenic flexure and is intraperitoneal (but the ascending and descending colons are mostly retroperitoneal)
Lateral to the ascending and descending colons is a space between the colon and posterior abdominal wall – called the left and right paracolic gutters (through which fluid/pus in the upper abdomen can trickle down into the pelvic cavity)
Clinical Anatomy of Rectum
The rectum is about 12 centimeters long and begins at the rectosigmoid junction, at the level of the third sacral vertebra or the sacral promontory. The rectum follows the shape of the sacrum and ends in an expanded section called the rectal ampulla. Unlike other portions of the colon, the rectum does not have taeniae coli
Supports of the rectum include
- The pelvic floor is formed by levator ani muscles
- Waldeyer’s fascia
- Lateral ligaments of the rectum which are formed by the condensation of pelvic fascia
- The rectovesical fascia of Denonvillers, which extends from the rectum behind to the seminal vesicles and prostate in front
- Pelvic peritoneum
- Perineal body
Clinical Anatomy Anal Canal
The anal canal below the pectinate line develops from ectoderm of the proctodeum,while that avobe the pectinate line develops from the endoderm of the hindgut.
The pectinate line is formed by the anal valves (transverse folds of mucosa) at the inferior-most ends of the anal columns. Anal glands open above the anal valves into the anal sinuses
The anal canal above the pectinate line is lined with columnar epithelium and below is lined with stratified squamous epithelium (transitional zone). The lower half of the anal canal (below the pectinate line) is divided into two zones separated by Hilton’s white line. The two parts are the zona hemorrhagic and zona cutanea, lined by stratified squamous-keratinized and stratified squamous keratinized, respectively. Anal columns (of Morgagni) are 6- 10 longitudinal (vertical) mucosal folds in the upper part of the anal canal
Clinical Anatomy of Vermiform Appendix
Embryologically, the appendix is a continuation of the cecum and is first delineated during the fifth month of gestation. The appendix does not elongate as rapidly as the rest of the colon, thus forming a wormlike structure. The appendix averages 10 cm in length but can range from 2-20 cm. The appendix is connected to the mesentery in the lower region of the ileum, by a short tube known as the mesoappendix
Short Medical Courses where Basic and Clinical Anatomy are studied
Paramedical 3 Years
Diploma Medical Assistant (DMA) 3 Years
Diploma in Medicine & Surgery (DMS) 3 Years
Diploma in Paramedical (DPM) 3 Years
Diploma in Medicine & Surgery (DMDS) 4 Years
Diploma in Medical Science (DMSc) 4 Years
All these Medical Courses are available at HRTD Medical Institute.
Veterinary Course where Basic and Clinical Anatomy are studied
Paramedical Vet ( Para Vet) 3 Years
Diploma Medical Assistant in Veterinary ( DMA Vet) 3 Years
Diploma in Medicine & Surgery in Veterinary ( DMS Vet) 3 Years
Diploma Paramedical in Veterinary ( DPM Vet ) 3 Years
Diploma in Medicine & Diploma in Surgery in Veterinary ( DMDS Vet ) 4 Years
All these Veterinary Courses are available at HRTD Medical Institute.
Sent
Enter
 Veterinary Training Course in Dhaka Pharmacy, Dental, Nursing, Veterinary, Physiotherapy, Pathology and Homeopathy training course
Veterinary Training Course in Dhaka Pharmacy, Dental, Nursing, Veterinary, Physiotherapy, Pathology and Homeopathy training course